What Is Liver Belly?
Liver belly, clinically known as abdominal distension or ascites related to liver conditions, refers to an abnormal enlargement of the abdomen due to the accumulation of fluid in the peritoneal cavity. This condition often manifests as a noticeable swelling in the abdominal area, which may feel tight or bloated. The presence of liver belly serves as an important symptom indicating potential underlying liver dysfunction or disease. It is essential to understand the role of the liver in the body’s overall functioning, particularly in digestion and metabolism, to comprehend why liver-related issues can lead to this condition.
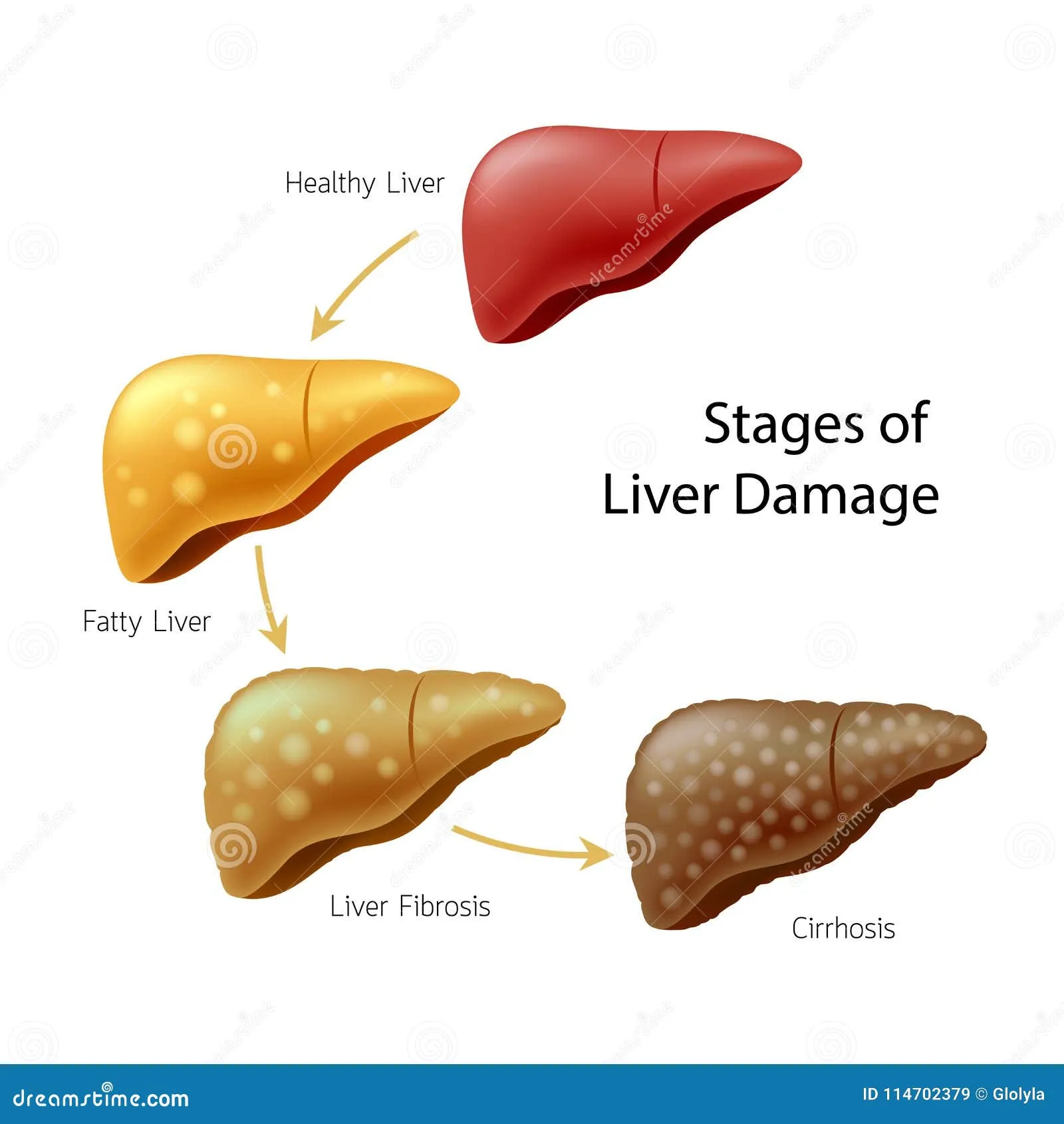
The liver plays a critical role in various metabolic processes, including the production of bile, detoxification of substances, and regulation of blood sugar levels. When the liver becomes compromised, its ability to perform these functions can be adversely affected, leading to a range of health complications. Liver diseases such as cirrhosis, hepatitis, and fatty liver disease can impair the organ’s functionality. As a result, fluid can begin to accumulate in the abdominal cavity due to increased pressure in the blood vessels surrounding the liver or reduced protein production by the liver, which is crucial for fluid balance.
Recognizing liver belly is significant, as it often serves as a warning sign of serious liver disease. Early detection of this symptom can lead to timely medical intervention, which is vital for improving the prognosis of liver-related conditions. A healthcare professional can perform a physical examination and recommend imaging tests to determine the underlying cause of the distension. Addressing the fluid buildup and its root cause not only aids in symptom management but also contributes to the restoration of normal liver function, enhancing overall health and well-being.
Causes of Liver Belly
Liver belly, also known as ascites, refers to the accumulation of fluid in the abdominal cavity, often resulting from underlying liver diseases. One of the primary causes is cirrhosis, which is the late stage of scarring (fibrosis) of the liver caused by various factors, including chronic alcohol abuse and viral hepatitis. As liver cells become damaged, their ability to function properly diminishes, leading to complications such as fluid retention and increased abdominal pressure.
Another significant contributor is non-alcoholic fatty liver disease (NAFLD). This condition involves the buildup of fat in liver cells, which can lead to inflammation and scarring. As NAFLD progresses, it may also result in liver dysfunction, contributing to the development of liver belly.
Hepatitis, an inflammation of the liver caused by viral infections, alcohol, or other factors, can also lead to ascites. Both acute and chronic forms of hepatitis can impair liver function, thereby sparking fluid accumulation in the abdomen. The impact of these liver conditions on fluid management in the body is critical, as a healthy liver is vital for processing and balancing bodily fluids.
Additionally, lifestyle choices play a crucial role in the development of liver belly. Heavy alcohol consumption markedly exacerbates liver disease and its associated complications. Obesity is another critical factor, with excess body weight contributing to metabolic disorders that place additional stress on the liver. Diets high in processed foods, sugars, and unhealthy fats further heighten the risk of liver damage, directly affecting liver functionality and potentially leading to ascites.
Symptoms and Diagnosis
Liver belly, often characterized by noticeable abdominal distension, is associated with several symptoms that can vary in intensity among individuals. One of the primary indications of this condition is abdominal swelling, which is often accompanied by a sensation of discomfort or even pain. Patients may experience a feeling of fullness, making it difficult to engage in regular activities such as eating or exercising. This fullness can also lead to significant changes in appetite, where an individual may either experience a reduced desire to eat or, conversely, an increased craving for food due to the perceived inability to satisfy hunger. In some cases, nausea or an overall feeling of malaise may also be present, further complicating diagnosis and management.
Timely detection of liver belly is crucial for effective treatment; hence, individuals exhibiting these symptoms should seek medical attention promptly. Healthcare practitioners utilize a multifaceted approach to diagnose the underlying issues contributing to liver belly. The initial evaluation typically involves a thorough physical examination, where the clinician assesses the abdomen for signs of swelling, tenderness, or any abnormal masses. Following the physical examination, imaging studies, such as ultrasounds, are employed to provide a clearer picture of liver health and to identify any structural abnormalities or fluid accumulation. These imaging techniques are invaluable in visualizing the liver’s condition, which is essential for accurate diagnosis.
Moreover, blood tests play a significant role in evaluating liver function. These tests measure various enzymes, proteins, and bilirubin levels, providing insights into the organ’s operational status. Abnormal results can indicate liver dysfunction or disease, helping healthcare providers formulate a comprehensive treatment plan. Thus, recognizing the symptoms and allowing for timely diagnosis through these methods are imperative steps in addressing liver-related complications effectively.
Treatment and Prevention Strategies
The management of liver belly, characterized by fluid accumulation due to various liver conditions, involves a multifaceted approach combining lifestyle adjustments, medical treatments, and potential surgical interventions. Initially, lifestyle changes are crucial in addressing the underlying issues that contribute to liver belly. A balanced diet rich in fruits, vegetables, whole grains, and lean proteins can significantly reduce fatty deposits in the liver. It is advisable to limit the intake of processed foods, sugars, and saturated fats. Hydration is also important, so individuals should aim to drink adequate water daily.
Regular physical activity plays a vital role in preventing and managing liver belly. Engaging in at least 150 minutes of moderate aerobic exercise per week can help improve liver function and reduce weight, which may alleviate fluid retention. Additionally, individuals should avoid excessive alcohol consumption, which can exacerbate liver damage. If alcohol use is a concern, seeking guidance from a healthcare professional can be beneficial.
Medical treatments for liver belly largely depend on the underlying cause. Medications may be prescribed to manage liver inflammation or treat infections. In some instances, diuretics are used to reduce fluid buildup; however, this should be done under a physician’s supervision. Should the condition progress significantly, surgical options, such as paracentesis, may be considered to remove excess fluid directly. This treatment provides temporary relief and serves as part of a broader management plan tailored to the individual’s needs.
It is essential for individuals experiencing symptoms of liver belly to consult healthcare professionals for personalized advice and tailored treatment plans. Addressing the root causes through comprehensive strategies not only aids in alleviating current symptoms but also helps prevent future complications associated with liver-related issues.